Table of Content
Please note that you typically pay a Medicare Part A deductible per benefit period before Medicare starts covering your inpatient hospital services. Aetna Medicare Advantage plans are required to cover one set of eyeglasses or contact lenses following a cataract surgery. This coverage requirement is in line with federal law that mandates Medicare Advantage plans meet the benefit minimums set forth by Original Medicare.

Many of Aetna’s regular medical plans cover the replacement of teeth due to a non-biting injury. Dental implants can sometimes be sought out for purely cosmetic reasons, so you may have to check with your plan to see if they will cover your specific implants and the reason why you’re getting them. Behavioral health, in many ways, is as important as physical health. Because of this, Aetna has extensive coverage for behavioral health programs. Aetna covers gender reassignment surgery if specific criteria are met. As of 2021, Aetna has begun to broaden its coverage for gender reassignment surgery to include breast augmentation surgery.
Best Dental Insurance For Seniors On Medicare Of 2021
Some Medicare Advantage plans provide further coverage for home health services, and this information should be included in your explanation of benefits. Everyone in Part B pays an insurance premium, and some people may pay more based on their income. Part B pays for some aspects of home health services, including medical equipment. CoverageHaven.com is owned & operated by Rank Media Insurance Agency LLC, a privately-owned non-government entity. Users seeking official government information can do so by accessing HealthCare.gov.

We offer discounts to help you save on a variety of health-related products and services. By partnering with CareLinx, Aetna will be able to address the needs of its aging members for affordable care in their own homes or communities. An Aetna Medicare plan can cover the cost of your transportation to a pharmacy or non-emergency doctor’s appointment using public transportation or a ride-sharing service. Some Aetna Medicare Advantage plans include memberships to the SilverSneakers fitness program which often include home exercise and nutritional programs. Covered social services can include counseling and other mental health and social support resources to address social or emotional conflicts interfering with one’s treatment or recovery.
Find Aetna Medicare Advantage Plans
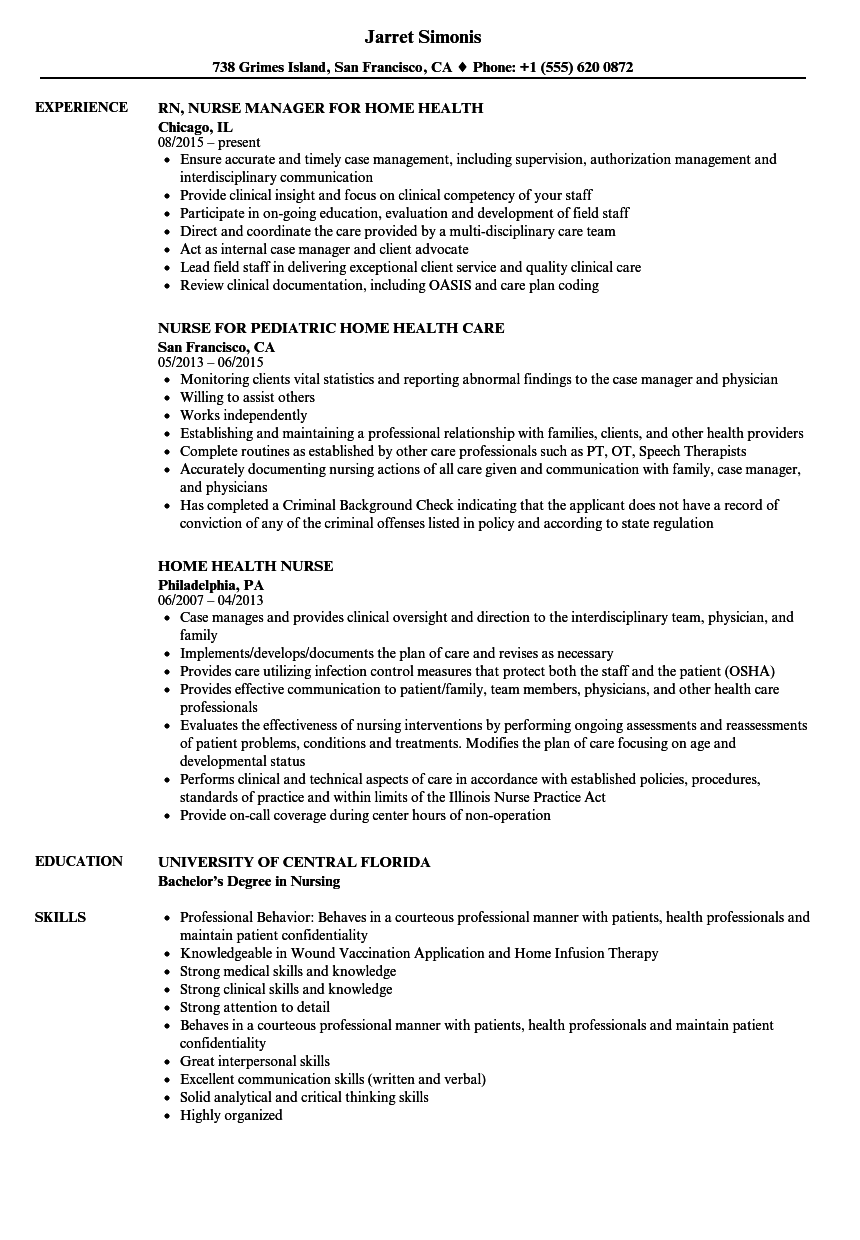
Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable. If your wisdom teeth are impacted, the treatment will likely fall under the dental surgery category and will be covered by your Aetna dental plan. Individual plans cap out at a maximum, and if you’re on an HMO plan, you’ll have to see your primary care practitioner to get a referral to a licensed psychologist. Allergy testing and desensitization injections can be a great way to determine allergies and prevent bad reactions if determined to be medically necessary by the Primary Care Physician.
Clinical Policy Bulletins are developed by Aetna to assist in administering plan benefits and constitute neither offers of coverage nor medical advice. This Clinical Policy Bulletin contains only a partial, general description of plan or program benefits and does not constitute a contract. Aetna does not provide health care services and, therefore, cannot guarantee any results or outcomes.
Will Medicare Pay For 24 Hour Home Care
Relax and recharge with discounts on massage therapy, acupuncture, chiropractic visits and nutrition services. It’s a nice perk that comes automatically with your Aetna benefits. Once you’re an Aetna member, just log in toyour member websiteto find participating professionals, order products and more. The Simple Steps To A Healthier Life®online health coaching programs let you choose the area of your health that you’d like to focus on. And they’re part of your health benefits, so it won’t cost you a penny.

If your pharmacy benefits are not with Aetna, contact your pharmacy benefits administrator for instructions. Check out our broader testing coverage frequently asked questions. Another option available through Aetna is the DentalFund plan which allows you to use untaxed dollars to pay your co-pays and out-of-pocket expenses. Preventive Services Task Force and the Centers for Disease Control and Prevention, Aetna recognizes HIV and Chlamydia testing as medically necessary.
This plan offers the most flexibility; however, services can often come with higher premiums and copays. Aetna is an insurance company that sells health coverage to millions of Americans across the country. The company was founded in 1853 and has since expanded to become one of the largest health insurance providers in the nation.

A Place for Mom’s in home health care services are completely free of charge for the elderly and their families here in Aetna. Their full range of plans has premiums ranging from $0 to over $100 each month, depending on your needs and location. If you choose United Healthcare, youll also receive access to additional AARP programs and services such as discounts on shopping and travel, savings on home and auto insurance, and free financial advice. NoteIf you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. Under this demonstration, your home health agency, or you, may submit a request for pre-claim review of coverage for home health services to Medicare. This helps you and the home health agency know earlier in the process if Medicare is likely to cover the services.
If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State or the Federal government. A home health aide is a provider who assists a member with non-skilled care to meet activities of daily living, thereby maintaining the individual in his or her home environment. Some Humana Medicare Advantage plans can cover home health care services such as care managers, home meal delivery, medical transportation, prescription drug deliver, caregiver support and more.
The home health agency should give you a notice called the Advance Beneficiary Notice" before giving you services and supplies that Medicare doesn't cover. Aetna Vision Preferred plan offers annual vision coverage for doctors in network; this typically includes a $0 annual vision test and other regular discounts on eyeglasses and contacts. Additional therapies and treatments are discounted through this insurance plan. Most Aetna plans cover therapy, often focusing coverage on evidence-based therapeutic services, such as psychoanalysis. It’s best to clarify coverage with your provider directly by phone.
According to studies, hearing loss that is not treated is cause for an average reduction of $12,000.00 in annual income. Hearing loss that is left untreated can also be linked to dementia, depression, hypertension, and an increased risk of falling. Using Medicares Find a Medicare Plan tool, you can log in without an account, choose a Medicare Advantage Plan, type in your ZIP code, and follow the simple instructions to get a list of the available plans. The Plan Details button helps you learn more about the coverage offered, such as preventative dental or comprehensive dental .
Learn more and find a Humana Medicare plan that offers the home health benefits you need. If your physician orders reasonable and medically necessary treatment of an illness or injury, Medicare will help pay for home health services as long as you meet certain criteria. To be eligible for home health services, your condition must be expected to improve in a generally predictable period of time. You may also qualify if you need a skilled therapist to safely and effectively create a maintenance program and to perform maintenance therapy for your condition. A registered nurse or licensed practical nurse may administer your home care which may include giving IV drugs, changing wound dressings, tube feedings, teaching about diabetes care, or certain injections. Private health insurance plans may pay for select elder care services, but coverage varies from plan to plan.

No comments:
Post a Comment