Table of Content
United Healthcare is our top overall pick for dental insurance for seniors on Medicare. They offer Medicare Advantage plans with an expansive network and flexible premiums. Aetna Medicare Advantage plans vary based on your location, but many plans offer opportunities to make access to your day-to-day necessities as simple as possible. During the COVID-19 pandemic, nurse practitioners, clinical nurse specialists, and physician assistants can provide home health services, without the certification of a physician. Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.

Although the housing cost charged by an assisted living facility will not be covered by Medicare, residents of assisted living homes can still benefit from Medicare coverage for certain services. Most health plans in the U.S. are subject to the new regulations that require them to cover the cost of at-home COVID tests. This includes employer-sponsored health plans as well as individual/family health plans that people purchase themselves . Medicaid and CHIP plans are also required to comply with the new regulations.
What States Offer Humana Medicare Advantage Plans
Some Medicare Advantage plans provide further coverage for home health services, and this information should be included in your explanation of benefits. Everyone in Part B pays an insurance premium, and some people may pay more based on their income. Part B pays for some aspects of home health services, including medical equipment. CoverageHaven.com is owned & operated by Rank Media Insurance Agency LLC, a privately-owned non-government entity. Users seeking official government information can do so by accessing HealthCare.gov.
So now more than ever, our in-home and online visits can be convenient, safe options for extra help managing your care. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. Therefore, Arizona residents, members, employers and brokers must contact Aetna directly or their employers for information regarding Aetna products and services.
Talk to a Licensed Insurance Agent
Participating providers are independent contractors in private practice and are neither employees nor agents of Aetna or its affiliates. Treating providers are solely responsible for medical advice and treatment of members. This Clinical Policy Bulletin may be updated and therefore is subject to change. While the Dental Clinical Policy Bulletins are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. The Dental Clinical Policy Bulletins describe Aetna's current determinations of whether certain services or supplies are medically necessary, based upon a review of available clinical information.
This plan offers the most flexibility; however, services can often come with higher premiums and copays. Aetna is an insurance company that sells health coverage to millions of Americans across the country. The company was founded in 1853 and has since expanded to become one of the largest health insurance providers in the nation.
Medigap Coverage Of Home Care Services
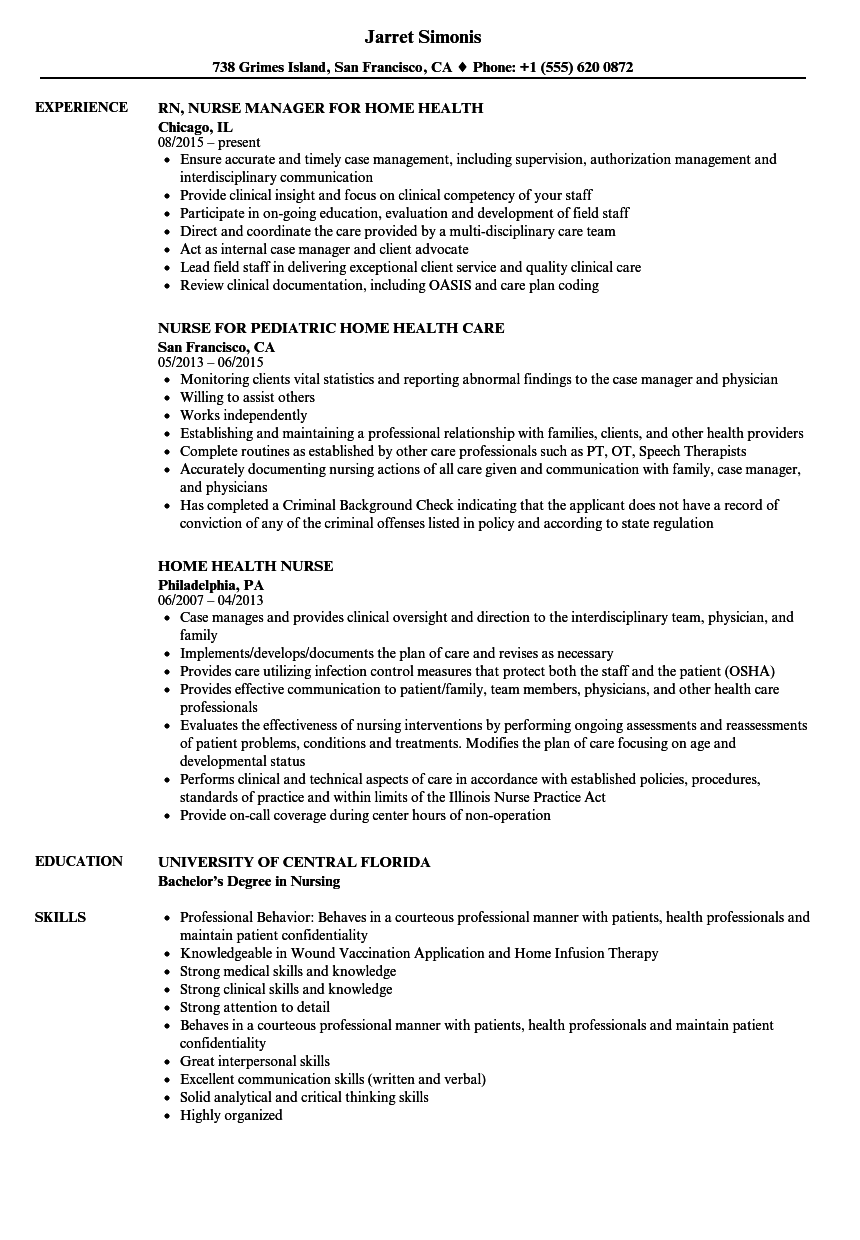
In-home services must come through a Medicare-approved Home Health Agency. Medicare covers in-home care for seniors with personal, hands-on care for an intermittent time. A home health care agency typically is the coordinator for any services your doctor orders. The prescription drug coverage that is offered by certain Humana PPO plans is equal to or even better than the standard requirement for Medicare Part D prescription drug plans. You actually employ the people who provide some of your home care services – they work for you .
According to studies, hearing loss that is not treated is cause for an average reduction of $12,000.00 in annual income. Hearing loss that is left untreated can also be linked to dementia, depression, hypertension, and an increased risk of falling. Using Medicares Find a Medicare Plan tool, you can log in without an account, choose a Medicare Advantage Plan, type in your ZIP code, and follow the simple instructions to get a list of the available plans. The Plan Details button helps you learn more about the coverage offered, such as preventative dental or comprehensive dental .
Home health services
If you have these plan types, you’ll likely need to get your home health services from an agency your plan specifically contracts with. Aetna Medicare members can get OTC COVID-19 tests from participating providers and pharmacies. You can find a partial list of participating pharmacies at Medicare.gov. Members should take their red, white and blue Medicare card when they pick up tests. They can also order up to two sets of four at-home tests per household by visitingCOVIDtests.gov.
Medicare’s home health benefit covers skilled nursing care and home health aide services provided up to seven days per week for no more than eight hours per day and 28 hours per week. If you need additional care, Medicare provides up to 35 hours per week on a case-by-case basis. Personal care is “non-skilled” care, or assistance with things like mobility, dressing, bathing, eating and toileting.
If you get a positive result, or if youre symptomatic and the at-home test shows a negative result, you may still want to follow up with your healthcare provider to schedule a PCR test. The government is working to make testing more readily available in these situations, too. Retrieved from /medicare/medicare-advantage-plans/humana-choice-ppo. This can include wheelchairs, walkers and other items and supplies that are used primarily in the home. Most Medicare beneficiaries have their choice of more than one Medicare Advantage plan where they live, and the coverage offered can differ in each plan.
Medicare Part A and Part B do cover some limited home health care services. A part-time home health care aide may be covered for a limited amount of time when certain conditions are met. In-home physical therapy, occupational therapy or speech-language pathology services can also be covered by Original Medicare. Coverage is good for a certain number of skilled nursing care hours per day and per week. Once a year during the Annual Enrollment Period , you can make changes to your Medicare coverage. Depending on which Medicare plan you have enrolled in, benefits can either be included in the plan’s premium or by paying an additional premium to get an optional supplemental benefit.
You may be able to choose to have either an allowance or a network benefit. With the allowance benefit you can visit any licensed health care provider for the service. You pay them directly and your insurance reimburses your allowance amount. If you choose a network benefit you get the service from a network health care provider and your insurance pays them directly.
Common chiropractic treatments include therapeutic exercise and stretching, spinal traction, and transcutaneous electric nerve stimulation , among others. You can take advantage of an in-person home visit — or an online virtual visit with the video and audio options that work best for you. The responsibility for the content of Aetna Clinical Policy Bulletins is with Aetna and no endorsement by the AMA is intended or should be implied.
Aetna is one of the most popular Medicare Advantage providers, with a clear focus on your overall well-being. Your doctor or other health care provider may recommend you get services more often than Medicare covers. Ask questions so you understand why your doctor is recommending certain services and if, or how much, Medicare will pay for them. Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare. Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services.

Thanks to new federal guidelines, you and everyone covered under your plan are eligible for eight at-home COVID-19 tests per 30-day period during the public health emergency. Just keep in mind that you need to have bought them on or after January 15, 2022, to be covered. Most plans will cover preventative treatments (like cleanings/check ups), basic treatments , and around 75% of coverage for treatments like root canals. Cosmetic procedures, like whitening or tooth shaping, are rarely covered by dental insurance plans – and, unfortunately, braces can fall under the cosmetic category.

No comments:
Post a Comment